We offer an individualized, multi-disciplinary approach to overcome symptoms of pelvic floor disorders. Our pelvic floor therapy offers innovative solutions for the following:
- Accidental bowel leakage
- Chronic constipation
- Pelvic organ prolapse
- Rectal cancer
Understanding The Pelvic Floor
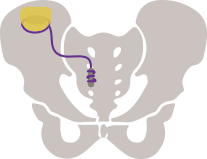
The pelvic floor consists of muscles, nerves and connective tissue that support the structures of the pelvis, including the rectum, bladder and female reproductive organs. Over time, or with acute injury, these supportive tissues may weaken, causing incontinence of urine and/or feces as well as vaginal prolapse.